 Scientific Editor: Editorial Board ISUD website
Scientific Editor: Editorial Board ISUD website
What is Open Prostatectomy?
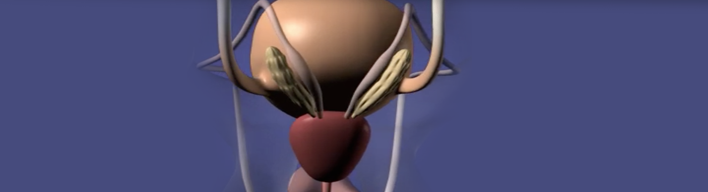
Open Prostatectomy is an open surgical intervention to remove the part of prostate that causes urinary obstruction. The prostate is accessed through a surgical incision that is made in the abdominal region.
When is Open Prostatectomy performed?
This procedure is indicated to treat symptoms caused by BPH (Benign Prostate Hyperplasia). It is a therapeutic option for patients who:
- do not respond to pharmacotherapy
- have experienced urinary retention (inability to urinate) more than once
- suffer from urinary overflow incontinence (i.e. incontinence due to bladder overfilling)
- suffer from recurrent urinary tract infections
- are predisposed to bladder stones or diverticula
- present hematuria (blood in urine), due to prostate size, that cannot be treated with pharmacotherapy
- present distention of the kidneys due to large post-void residual urine volume, that may potentially affect renal function
Open Prostatectomy is usually performed when the prostate volume is large (over 80ml) and therefore the procedure cannot be conducted thransurethrally.
What sort of preparation is required?
Upon hospital admission, preoperative preparation includes blood tests, chest X-ray and ECG (electrocardiogram). In case you are on anticoagulants, it may be required to interrupt your anticoagulant therapy a few days before the operation. You should always consult your Cardiologist, for there may be need to replace anticoagulants with injections in the abdominal region.
How is the procedure performed?
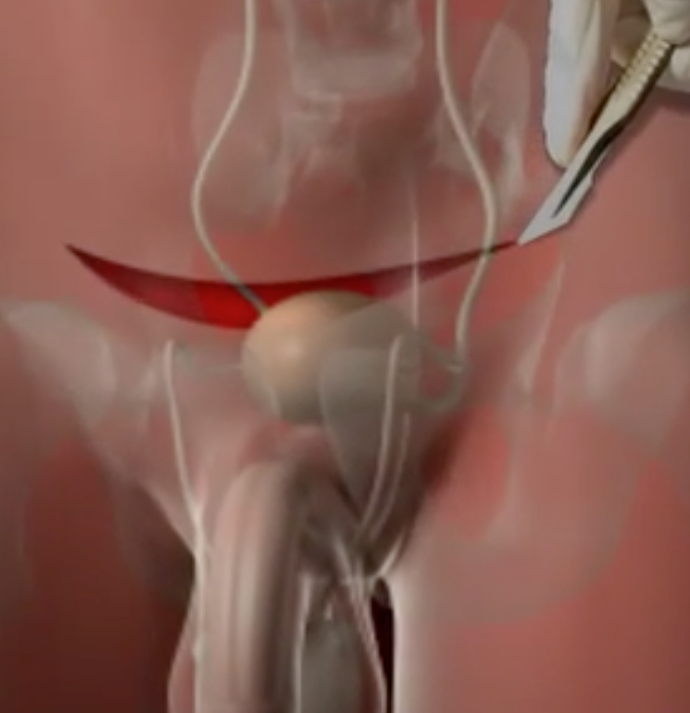
Open Prostatectomy is performed either under general anesthesia (with patient sleeping throughout the procedure) or under spinal anesthesia (with patient being awake during the procedure but feeling no pain from waist down). The procedure usually lasts 45-60 minutes. An incision is made in the abdomen below the umbilicus for accessing the prostate and removing that part which is hyperplastic and creates urinary obstruction. There are two methods of open prostatectomy giving the same results. Their difference lies in the fact that in one method the prostate is removed through the bladder, whereas in the other method the prostate is accessed and removed directly through an incision that is made upon the prostate. At the end of the procedure, a catheter is placed to the bladder through the urethra. The bladder catheter is removed on postoperative days 6-8. The average hospital stay is usually 7-10 days. The surgical stitches will be removed from the skin incision on postoperative days 7-10.
What about after the procedure?
Upon discharge from hospital, you will given specific written instructions about:
- when it is safe to restart your anticoagulant therapy
- when it is safe to resume to intense physical activity and work
- what antibiotic regimen you will have to take after the operation
You should be aware that urine will have a pinkish color for some time after surgery. You should drink plenty of fluids. You may also present urinary frequency and urgency, symptoms that will gradually subside.
What is the effect of the procedure on patient’s life?
Most patients face no problem after the surgery. Prostatectomy does not usually affect the patient’s sexual life, as long as erectile function had been normal before surgery. As soon as you feel comfortable (usually 3-4 weeks after surgery), you can resume to your sexual activities.
In most cases, patients will have no ejaculation during orgasm. This is called retrograde ejaculation, i.e. semen is redirected back to the bladder and eliminated through urine instead of going out through the urethra during ejaculation. Patients who are interested in having children in the future should be aware of this.
You may feel intense urinary frequency and urgency, and sometimes urinary incontinence, which may take up to 3 months to improve. Lastly, it is important to seek the histological result; should it reveal prostate cancer that could not be diagnosed preoperatively, there may be need for further therapy.