- Cystocele, Rectocele, Uterine Prolapse
- What is a Cystocele?
- What are the causes of Cystocele?
- What are the symptoms in Cystocele?
- How is Cystocele diagnosed?
- How is Cystocele treated?
- What is a Rectocele?
- What is Uterine Prolapse?
Cystocele, Rectocele, Uterine Prolapse
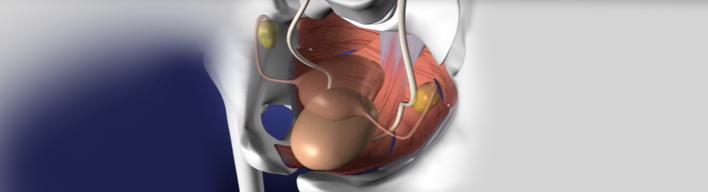
These three conditions are often referred to altogether as "Pelvic Organ Prolapse" (POP), as bladder, rectum and uterus are all anatomically located in the pelvis (basin). They are particularly common conditions occurring in about 1 out of 12 women, while they may be identified during gynecological examination in 1 out of 3 women over 50 years old.
Below follows a more analytical presentation of these conditions and mainly of Cystocele, which is the most common of the three.
What is a Cystocele?
Cystocele -also known as Prolapsed Bladder or Fallen Bladder- is the condition when the bladder descends (drops) lower than its normal position within the vagina; the bladder bulges out or protrudes into the vagina. In milder cases, the bladder descends down to the virgin hymen right before the vaginal entrance. In more severe cases, the bladder may even protrude out of the vagina as a soft mass.
What are the causes of Cystocele?
Cystocele is formed due to the loosening of muscles and ligaments supporting and retaining the bladder in its normal position. Today we are aware that there are many predispository factors that may result in its formation: multiple normal birth deliveries, high birth weight, long duration of normal delivery, difficulty of normal delivery, instrumentation for extracting the baby from the vagina; obesity, normal hormone deficiency with age advancement, heavy physical work; chronic cough (induced by smoking, allergies), chronic constipation.
Cystocele may also exacerbate when following a Hysterectomy (surgical removal of the uterus). Lastly, it is believed that also genetic factors predispose for its formation.
What are the symptoms in Cystocele?
The most common symptom is feeling heaviness in the vagina, usually observed in advanced stage cystocele. In such cases, there may be vaginal trauma and hemorrhage causing problems to sexual activity, and sometimes may even cause problems in walking. A large cystocele may cause difficulty to urinate and inability of complete voiding of the bladder; as a result, there may be urinary tract infections due to stagnant urine. In exceptionally rare cases, the inability of the bladder to normally void may cause renal problem.
How is Cystocele diagnosed?
You have to be physically examined by your physician -either Gynecologist or Urologist- in a gynecological position. You will be asked to cough or tighten your abdomen. S/he will check whether the bladder is localized in the vagina and whether there is leakage of urine, i.e. incontinence. Large grade cystoceles are visible even with plain physical examination. You may be asked to urinate and then undergo ultrasound screening, to find out whether your bladder voids properly. In some cases, some extra radiological examinations, such as Cystography, or MRI have to be done, so that the physician gets as much information as possible.
How is Cystocele treated?
Severe cystocele cases can be treated only surgically. There are no drugs that can relocate the bladder to its normal position. During surgical repair, the bladder goes back to its normal position and is fixated there, either by being simply sutured or by inserting a special mesh. Before resorting to surgery, a temporary solution often tried is placing a ring high into the vagina (a vaginal 'ring pessary', as it is called). This ring pessary aims at supporting the bladder in its proper position for about 6 months, so that both the patient and her physician get an idea of how the patient's micturition condition will be postoperatively. This is necessary to be done because very often a cystocele hides a urinary incontinence that is manifested after surgery.
Moderate cases are operated only when the cystocele causes serious life-quality problems to the patient.
Special physiotherapeutic exercises for strengthening the muscles supporting the bladder and genitalia, could help in mild cystocele cases.
What is a Rectocele?
Rectocele -also known as Rectal Prolapse- is the condition when the ending of the large intestine (rectum) pushes the back wall of the vagina. In most severe rectocele cases, the rectum may even slide out of the vagina. Etiology and symptoms are similar to those of cystocele. Severe rectocele may cause problems to defecation and sexual intercourse. Rectocele is diagnosed in the same way as cystocele. Severe rectocele cases can be treated only surgically.
What is Uterine Prolapse?
Uterine Prolapse is the condition when the uterus (womb) drops down from its normal position into the vagina. In most severe cases, the cervix (neck of the uterus) may extend so far that it actually comes out of the vaginal opening, and Gynecologists usually have to remove the uterus.
When bladder, rectal and uterine prolapse coexist, surgical repair by specialized surgeons is necessary and feasible.