Scientific Editor: Editorial Board ISUD website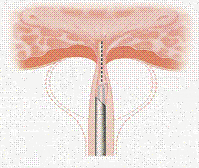
- When is Bladder Neck Incision (BNI) performed?
- What sort of preparation is required?
- How is the procedure performed?
- What about after the procedure?
- What is the effect on patient’s quality of life?
When is Bladder Neck incision (BNI) performed?
BNI is a surgical procedure to treat symptoms when urine has difficulty passing through the bladder neck and, as a result, there is inability to urinate properly (bladder neck is the last part of the bladder before the urethra).
The causes that might result in such symptoms are:
- Bladder neck obstruction (including idiopathic bladder neck obstruction and neurological diseases that cause blockage of the bladder neck when urinating).
- Bladder neck stenosis, usually occurring after surgical operations in the region. Such common examples are radical prostatectomy, transurethral prostatectomy (TUR-P) etc.
- Benign prostate hyperplasia (BNH). The BNI method gives equal results to TUR-P when performed for prostate tumors <30ml.
What sort of preparation is required?
Upon hospital admission, preoperative preparation includes blood tests, chest X-ray and ECG (electrocardiogram). In case you are on anticoagulant therapy, it may be required to interrupt your anticoagulant therapy a few days before the operation. You should always consult your Cardiologist, for there may be need to replace anticoagulants with injections in the abdominal region.
How is the procedure performed?
The procedure requires general or spinal anesthesia. In the beginning, the patient is positioned in the gynecological examination position, the region is cleansed and the urethra lubricated. A mini camera is inserted through the urethra to locate the bladder neck. With the use of an instrument attached to the camera, one or two incisions are made in the bladder region. Then, the incised area is cauterized to prevent bleeding. At the end of the procedure, a catheter is placed for applying continuous bladder irrigations with normal saline.
Hospital stay is about 2 days. The catheter is usually removed on postoperative day 2. Alternative surgery is BNI with the use of laser technology. Studies have shown that this is the appropriate method for patients who are on anticoagulant treatment, for it reduces hemorhage risk.
What about after the procedure?
During the first postoperative days, the patient may feel a burning sensation in the urethra and present blood in the urine (hematuria). Also, the catheter may cause bladder spasm and intense pain, which lasts though only a few seconds. These symptoms can improve with appropriate pharmaceutical agents. When hematuria occurs, the catheter is kept and continuous bladder irrigations are applied for as long as required.
Once the catheter is removed, the patient’s urinary function is checked. An ultrasound is performed to make sure there is no post-void residual urine (i.e. no urine left in the bladder after voiding).
Upon discharge from hospital, you will be given specific written instructions about::
- what antibiotic regimen to take
- how long to abstain from physical strain
- how important it is to drink plenty of fluids
You should necessarily consult your Cardiologist about when to restart your previous anticoagulant treatment.
What is the effect on patient’s quality of life?
Most patients face no problem after the procedure. More than half of the patients will present absence of ejaculation. This occurs because, once the prostate is resected, semen does not get ejaculated normally through the urethra but goes back into the bladder (retrograde ejaculation) and is eliminated with urine.
With regard to nutrition after surgery, you should take about 1.500ml fluids daily and avoid coffee, alcohol and smoking, for they may cause irritative symptoms.


