Scientific Editor: Editorial Board ISUD website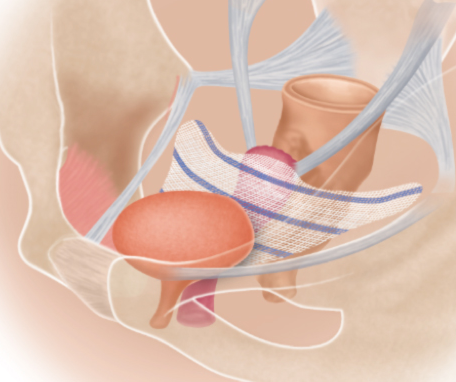
- What is a Transvaginal Mesh (TVM)?
- When is it placed?
- What sort of preparation is required?
- How is it placed?
- What about after placing it?
- What is the effect on patient’s quality of life?
What is a Transvaginal Mesh (TVM)?
Transvaginal mesh (TVM) is a synthetic mesh that is placed at the anterior vaginal wall of the patient to prevent vaginal wall prolapse.
When is it placed?
Not every cystocele (vaginal prolapse) is necessarily an indication for placing TVM. Indications for the transvaginal placement of a synthetic mesh include: incomplete bladder voiding (i.e. post-void residual urine), severe vaginal prolapse and urinary incontinence. Dyspareunia (vaginal pain during sexual intercourse) is not an absolute indication, for it does not always improve after the procedure.
What sort of preparation is required?
Upon hospital admission, preoperative preparation includes blood tests, chest X-ray and ECG (electrocardiogram). In case you are on anticoagulant therapy, it may be required to interrupt your anticoagulant therapy a few days before the operation. You should always consult your Cardiologist, for there may be need to replace anticoagulants with injections in the abdominal region.
How is it placed?
The surgical procedure requires general or spinal anesthesia. In the beginning, the patient is placed in the gynecological examination position, the region is cleansed and a catheter is placed in the bladder. The transvaginal mesh is inserted through an incision that is made at the anterior vaginal wall, in order to provide support and prevent the prolapse or bulging of the bladder into the vagina. At the end of the procedure, some gauze is placed in the vagina to act as a bandage for the first 24 hours and is removed the next day. Hospital stay is about 2 days. The catheter is usually removed on the first postoperative day.
Perioperative complications are very rare. These may be either urethral or bladder injury, which can be restored with immediate stitching and keeping the catheter longer. Other rare complications are tissue erosion and mesh rejection.
What about after placing it?
During the first postoperative days, the patient may feel a burning sensation in the urethra. Also, the catheter may cause bladder spasm and intense pain, which lasts only a few seconds but recurs at regular time intervals. These symptoms can improve with appropriate pharmaceutical agents.
Once the catheter is removed, the patient’s urinary function has to be checked. An unltrasound is performed to make sure there is no urine left in the bladder after voiding.
Upon discharge from hospital, you will be given specific written instructions about::
- what antibiotic regimen to take
- how long to abstain from physical strain
- how important it is to drink plenty of fluids
You should necessarily consult your Cardiologist about when to restart your previous anticoagulant treatment.
What is the effect on patient’s quality of life?
Most women do not face any problem after having a transvaginal mesh placed. With regard to nutrition, you should receive about 1.500ml fluids/ day and avoid coffee, alcohol and smoking, for they may cause irritative symptoms.


