Dermatological diseases of the external genitalia in men and women may be either sexually transmitted or non-sexually transmitted.
Although there is relatively high public awareness and frequent editions of relevant guidelines, such as Sexually Transmitted Diseases Treatment Guidelines (2010) the issue remains a headache for Urologists who have to treat patients who seek their advice. It is with great pleasure that ISUD is presenting this concise Atlas of Genital Dermatological Conditions, which was compiled by the most competent specialists, i.d. the staff of the Special Department of Genital Dermatological Diseases of Papageorgiou Hospital in Thessaloniki This special department was created in 2010 and resulted from the cooperation of the 2nd University Clinic of Dermatological and Sexually-Transmitted Diseases (Director: Prof. D. Sotiriadis) and the 2nd Unorology Clinic of AUTh (Director: Prof. E. Ioannidis). This Atlas emerged from the training offered by Prof. D. Sotiriadis at the 4th Interactive School of Urology.The Tables and Pictures present in a particularly concise manner common and rare dermatological diseases of the genitals.
The Editorial Committee of the Atlas was composed of:
- Dimitris Sotiriadis, Prof. of Dermatology, AUThProf. of Dermatology, AUTh
- Dimitris Kalabalikis, Lecturer of Dermatology, AUTh
- Nikos Koliakos, Urologist, Scientific Associate of the 2nd Urology Clinic of AUTh
|
Sexually-Transmitted Diseases |
Non-Sexually Transmitted Diseases |
|---|---|
|
|
|
|
|
Condyloma Acuminatum
Herpes Simplex
|
Cause |
Caused by HSV 2 and HSV 1 |
|
Transmission |
Direct contact with active lesion or biological fluid containing the virus (Sexually-transmitted disease) |
|
Clinical Picture |
Precursor symptoms (burning sensation - itching), Bubbles on red blotchy-oedematous base which develop into an erosive lesion |
|
Diagnosis |
Visually, through clinical examination |
|
Incubation period |
3-7 days |
|
Differential Diagnosis |
Syphilis, injuries, ulcers, pharmacogenic rash, mucus membrane pemphigoid |
|
Treatment |
Anti-herpes medication: quite effective if administered in good time (within the first 48-72 hours) |
|
Comments |
Spontaneous remission within 1-2 weeks; Frequent recurrences; Recurrent herpes: milder symptoms |
| Photographs available: |
Molluscum Contagiosum
|
Cause |
Viral infection – small pox type viruses (MCV -1, MCV - 2). MCV-2 most prevalent among AIDS patients |
|
Transmission |
Infection through contact (sexual or other) |
|
Clinical Picture |
White-yellow, dome-shaped bumps |
|
Diagnosis |
Visually, with clinical examination |
|
Incubation period |
15 days - 6 months |
|
Differential Diagnosis |
Folliculitis, condyloma acuminatum, warts, milia |
|
Treatment |
Destruction of lesion (crushing, cryopexy, diathermy) |
|
Comments |
Spontaneous self-limiting within 6-9 months, although successive exposure due to self-inoculation may be a problem |
| Photographs available: |
Eczema - Contact Dermatitis - Seborrheic Dermatitis
|
Cause |
Self-immune disease – there is hereditary predisposition |
|
Transmission |
Non-transmitted |
|
Clinical Picture |
Erythematous, erosive lesions; itching, lichenisation |
|
Diagnosis |
Visually, with clinical examination. Persistent in taking history. (sensitive to detergents, cosmetics, latex, treatment products!!) |
|
Incubation period |
- |
|
Differential Diagnosis |
From almost everything else |
|
Treatment |
Avoidance of triggering cause– corticosteroids |
|
Comments |
Seborrheic - atopical (history) |
| Photographs available: |
Lichen Planus
|
Cause |
Unknown aetiology (immunomediated, Τ - lymphocytes.) |
|
Transmission |
Non-transmitted |
|
Clinical Picture |
Labia majora, labia minora, penile body, prepuce, balanus; Red-blue / red-violet blotches, occasionally ring-like, shining or erosive lesions (mainly in women), Hypertrophic/ hyperkeratotic (rarely...) |
|
Diagnosis |
Visually, with clinical examination; Biopsy |
|
Incubation period |
-- |
|
Differential Diagnosis |
Lichen sclerosus, psoriasis, scabies, eczema |
|
Treatment |
Corticosteroid and immunomodifiers; Spontaneous remission. |
|
Comments |
Genitalia affected in 50% of women and 35% of men with Lichen planus |
| Photographs available: |
Lichen Sclerosus et Atrophicus - Balanitis xerotica obliterans( men) - Kraurosis Vulvae (women)
|
Cause |
Unknown aetiology (idiopathic, inflammatory) |
|
Transmission |
Non-transmitted |
|
Clinical Picture |
Hypochromasia, sclerosis – atrophy, erosive lesions - itching (women), Paraphimosis - phimosis – stenosis of external urethra orifice (men), Painful erections |
|
Diagnosis |
Visually, with clinical examination. Biopsy |
|
Incubation period |
- |
|
Differential Diagnosis |
Erosive Lichen planus, Queyrat Erythroplasia, Cicatricial pemphigoid, Eczema (vaginal) |
|
Treatment |
Local corticosteroids combined with cicatrizants and Vitamin E per os. |
|
Comments |
Women / men — — 10/1, increases with age, mainly among non-circumcised individuals, but not only. |
| Photographs available: |
Zoon' s Balanitis - Balanitis Plasmacellularis/ Vulvitis
|
Cause |
Unknown aetiology (not among circumcised individuals!) |
|
Transmission |
Non-transmitted |
|
Clinical Picture |
Erythematous (" red pepper" ) wet, well circumscribed plaques. Mild erosion (?) Usually asymptomatic |
|
Diagnosis |
Visually, with clinical examination, Histological examination (necessary): zonary, plasmatocyte infiltration below the epithelium |
|
Incubation period |
- |
|
Differential Diagnosis |
Lichen, Cicatricial pemphigoid, extramammary Paget’ s disease (EMPD) |
|
Treatment |
Mild corticosteroids, immunomodifiers, meticulous local hygiene |
|
Comments |
Overwhelmingly more frequent among men ( > 30 years of age) |
| Photographs available: |
Freckles - Naevi - Stable Pharmacogenic Rash
|
Cause |
Pharmaceutical aetiology (pharmacogenic) |
|
Transmission |
Non-transmitted |
|
Clinical Picture |
Single or several lesions, round or oval, grey-black or blue-grey in colour |
|
Diagnosis |
Visually, with clinical examination. History is of the essence |
|
Incubation period |
- |
|
Differential Diagnosis |
Malignant melanoma |
|
Treatment |
Avoidance of the medication that caused it (in pharmacogenic rash cases.) |
|
Comments |
- |
| Photographs available: |
Pemphigoid Vulgaris
|
Cause |
Self-immune, relatively rare dermatopathy |
|
Transmission |
Non-transmitted< |
|
Clinical Picture |
Often appears in semi– mucous membranes; Very rarely only in the genitalia. Erosive – ulcerative lesions on the balanus, the labia and the entrance to the vagina. |
|
Diagnosis |
Visually, with clinical examination, Tzanck (+) Cytological examination, histological examination. |
|
Incubation period |
-- |
|
Differential Diagnosis |
All cases with erosive lesions |
|
Treatment |
Systemic corticosteroids and immunosuppressant treatment |
|
Comments |
Cautious prognosis |
| Photographs available: |
Candidiasis
|
Cause |
Usually Candida albicans (fungus)) |
|
Transmission |
Usually – but not always – sexually transmitted. |
|
Clinical Picture |
Erythema, whitish-thick secretion (not urethral), erosive lesions, oedema |
|
Diagnosis |
Visually, with clinical examination. |
|
Incubation period |
1-3 days |
|
Differential Diagnosis |
Seborrheic eczema, Contact dermititis, Cicatricial pemphigoid |
|
Treatment |
Local antifungal treatment sufficient |
|
Comments |
Higher incidence among diabetics, immunosuppressed patients or following antibiotic treatment |
| Photographs available: |
Scabies/ Phthirus Pubis (parasites)
|
Cause |
Scabies mite / pubic lice |
|
Transmission |
Through contact (sexual or other) |
|
Clinical Picture |
Scabies: typical scabies rash in the male genitalia (blotches, tunnels), Lice: finding the lice- nits in the pubic region |
|
Diagnosis |
Visually, with clinical examination. |
|
Incubation period |
Scabies: 2-4 weeks |
|
Differential Diagnosis |
Local treatment sufficient |
|
Treatment |
Local anti-fungal treatment sufficient |
|
Comments |
Intense itching not responsive to anti-histamine medication |
| Photographs available: |
Syphilis (parasites)
|
Cause |
Treponema pallidum (Spirochoeta pallida) (NOT cultivated) |
|
Transmission |
Sexually but also vertically transmitted disease |
|
Clinical Picture |
Usually single painless lesion, round or oval, with smooth borders, clear floor and the appearance of ‘ muscular flesh’ seated on a hard base |
|
Diagnosis |
Try to find the Treponema pallidum, dark field microscopy, direct immunofluoresence, trying to find antibodies, non-specific serological reactions (RPR, VDRL), specific serological reactions (FTA abs, TPHA) |
|
Incubation period |
21 days |
|
Differential Diagnosis |
herpes, injuries, ulcers, pharmacogenic rash |
|
Treatment |
Parenteric administration of penicillin |
|
Comments |
Ipsilateral painless lymphadenitis (sentinel lymph node). The ulcer recedes without treatment after 4-6 weeks. ‘ Any lesion of the genitals is SY, until proven otherwise’ . |
| Photographs available: |
Penile Pearls
|
Cause |
Hypertrophic growth from the semi-mucous membreane of the balanus |
|
Transmission |
Non-transmitted |
|
Clinical Picture |
Semi-spherical or conical blotches, about 1mm in diameter and height, arranged in 1-3 rows in the balanus corona region, partially or fully surrounding it. |
|
Diagnosis |
Visually, with clinical examination. The blotches are whitish-pink, red-pink or normal mucosa colour; Elastic in texture and asymptomatic. |
|
Incubation period |
-- |
|
Differential Diagnosis |
Condyloma acuminatum |
|
Treatment |
Not necessary |
|
Comments |
Normal condition noted in the balanus corona region after puberty |
| Photographs available: |
Bowenoid Papulosis
|
Cause |
HPV 16, 18 |
|
Transmission |
Sexually transmitted disease |
|
Clinical Picture |
Flat brown-grey or red-violet papillas with a smooth surface; 2-4 mm. |
|
Diagnosis |
Visually, with clinical examination. Biopsy: Bowen Disease histological findings |
|
Incubation period |
-- |
|
Differential Diagnosis |
Condyloma acuminatum, Warts, Naevi |
|
Treatment |
Lesion destroyed with Cryopexy, Diathermy coagulation, Laser CO2 |
|
Comments |
This is an endothelial neoplasia |
| Photographs available: |
Queyrat Erythroplasia
|
Cause |
Associated with HPV 16 (as well as other HPV viruses) |
|
Transmission |
Unknown whether included in STD. |
|
Clinical Picture |
Erythematous – shining plaques, erosive lesions |
|
Diagnosis |
Visually, with clinical examination; biopsy |
|
Incubation period |
-- |
|
Differential Diagnosis |
Lichen sclerosus, Lichen Planus, Zoon’ s Balanitis |
|
Treatment |
Local excision, imiquimod, 5FU, photodynamic |
|
Comments |
This is an endothelial neoplasia (Acanthocytes in situ) |
| Photographs available: |
Squamous Cell Carcinoma
>
Malignant Melanoma
|
Cause |
Unknown |
|
Transmission |
Not transmitted |
|
Clinical Picture |
Rarely located in the genitals - Non-melanoma types: 25% |
|
Diagnosis |
Biopsy is compulsory if there is a suspicious lesion |
|
Incubation period |
-- |
|
Differential Diagnosis |
Naevi, seborrheic warts, ‘ benign’ lesions (for non-melanoma type) |
|
Treatment |
Excision to healthy borders |
|
Comments |
Exceptionally negative prognosis |
| Photographs available: |
Other more rare lesions diagnosed during the operation of the Department.
Fibroepithelial Polyp
|
Comments |
Skin lesion located in the coronary sulcus; soft in texture and asymptomatic; It was excised. |
|
Histological Diagnosis |
Fibroepithelial polyp; Benign aetiology. |
| Photographs available: |
Urethra Ectropion
|
Comments |
Reddish nodule projecting from the outer urethra orifice; It causes mild haematuria. It was excised. |
|
Histological Diagnosis |
Urethra ectropion. |
| Photographs available: |
Reverse Acne in the Perigenital Region
|
Comments |
Confluent nodule-cystic lesions and small blisters located in the perigenital region. Biopsy was performed. The lesions subsided when treated with antibiotics locally and per os. |
|
Histological Diagnosis |
Reverse acne |
| Photographs available: |
Seborrheic Scrotal Cysts
|
Comments |
Multiple scrotal nodules, hard and painless. |
|
Histological Diagnosis |
Seborrheic scrotal cysts |
| Photographs available: |
Inflammatory Balanus Ulcer due to Phimosis
|
Comments |
Elderly patient with neglected phimosis presenting intense inflammation. Circumcision was performed. The balanus presented deep, painless ulcer. Biopsy of lesion specimens showed no malignancy. |
|
Diagnosis |
Inflammatory ulcer. |
| Photographs available: |
Folliculitis
|
Comments |
Multiple follicular lesions located on the balanus and the prepuce, caused by excessive use of corticosteroids. Local antibiotics were administered; Lesions disappeared completely. |
| Photographs available: |
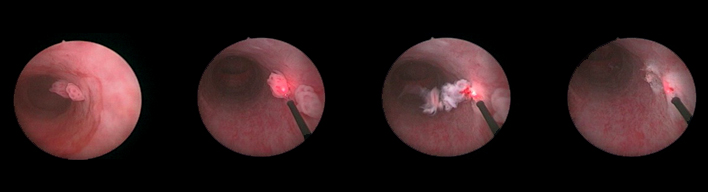
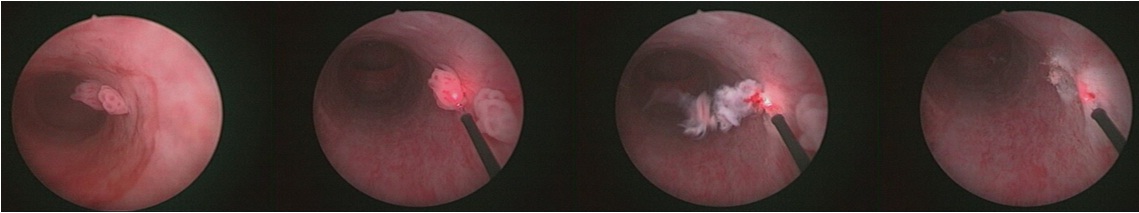
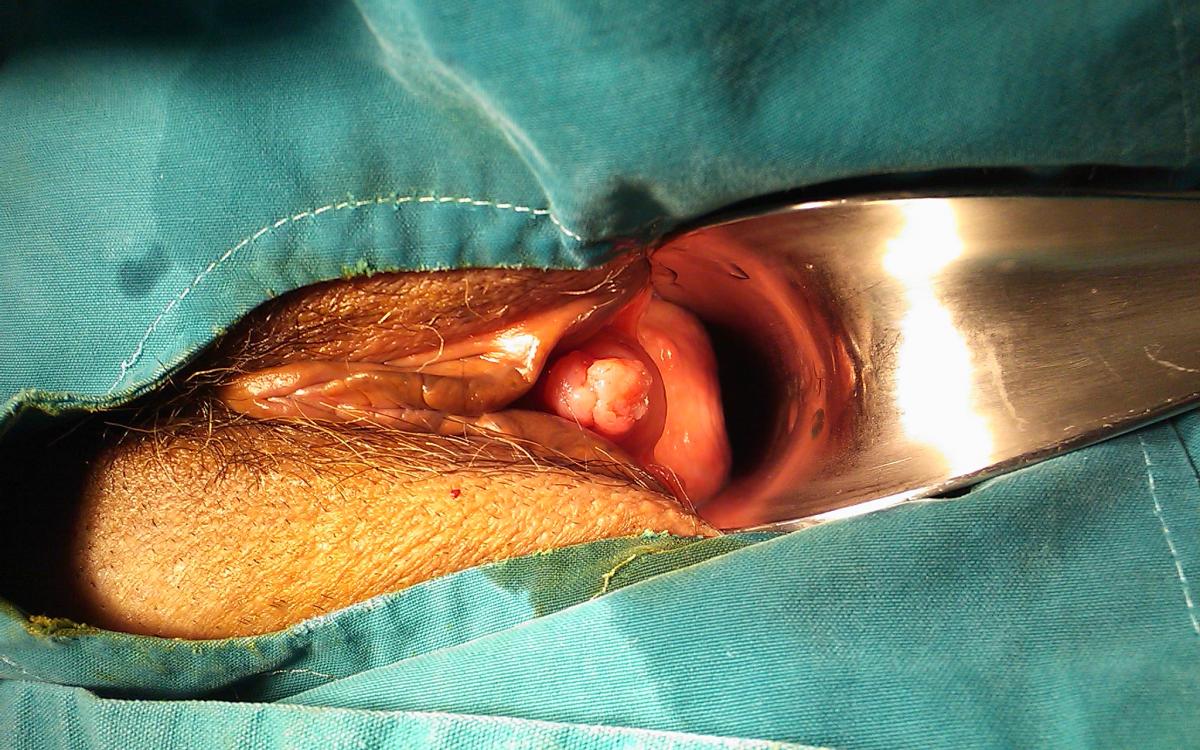
Pyogenic Granuloma
|
Comments |
Red nodule, soft in texture with a constricted base; Painless; Micro-haemorrhaging when pressed. It was excised and biopsy was performed. |
|
Histological Diagnosis |
Pyogenic granuloma. Recurrence of lesion; patients underwent diathermy coagulation and cryotherapy. |
| Photographs available: |