- Interstitial Cystitis - Bladder Pain Syndrome (IC/ BPS)
- How are IC/ BPS diagnosed?
- Is there treatment for IC/ PBS?
- What is the Chronic Pelvic Pain Syndrome?
- Is there treatment for the Chronic Pelvic Pain Syndrome?
Interstitial Cystitis - Bladder Pain Syndrome (IC/BPS)
The medical term 'syndrome' is defined as a set of problems observed in several patients, which are though of unknown or unclear etiology, since many different conditions or diseases could induce the same symptoms. In Bladder Pain Syndrome (BPS), the most common symptoms are pain experienced during the bladder filling phase (with pain temporarily relieving after urination), feeling of heaviness in the bladder and constant urge to urinate, urinary frequency with small amounts of urine and nocturia (need to frequently wake up in the night to urinate). The pain is often localized in the urethra or low adbdomen. Symptoms persist for at least one year. Interstitial Cystitis (IS) is a rare and more severe form of Bladder Pain Syndrome. BPS and IC are more common in women compared to men. In general, they are rare conditions. In Europe there are less than 20 cases/100.000subjects, while in America there are up to 60 cases/100.000 subjects. However, symptoms may significantly affect the patients' quality of life. Almost half of women with Interstitial Cystitis, suffer from depression due to the above problem.
How are IC/ BPS diagnosed?
The diagnosis of Interstitial Cystitis presupposes that we have first excluded any other pathological condition originating from pelvic organs, i.e. urological, gynecological or intestinal disease. For example, a stone in the bladder may cause similar symptoms during urination without having the diagnosis of BPS. Also, patients are often treated for potential urinary tract infections because pyospheres have been identified in their urine, even though urine culture has identified no bacteria.
For IC diagnosis, a special endoscopy (Cystoscopy) is performed, during which the physician fills up the bladder with sterile water. This is usually done with the patient under general anesthesia. In the most severe cases, there are even ulcerations and hemorrhagic foci within the bladder. During cystoscopy, bladder specimen is obtained for biopsy that will show whether there are any specific cells or whether it is a condition of chronic inflammation.
Is there treatment for IC/BPS?
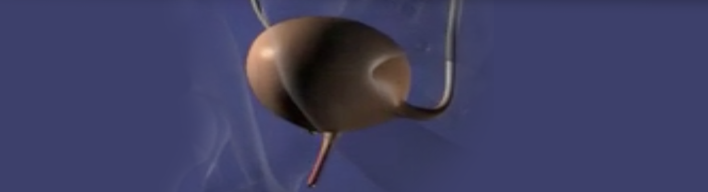
In general, the treatment is difficult, for the etiology of the disease is not yet clear. Patients usually try different therapeutic options -mainly antibiotics- without success in alleviating their symptoms. Antihistamines, antidepressants, some immunosuppressants and infusion of specific fluids into the bladder have demonstrated improvement of patients' symptoms. Antiinflammatory drugs do not seem to be effective despite the fact there is usually chronic inflammation in the bladder. During the last years, quite successful is the use of neurostimulation through the spine and Botox injection in the bladder. In severe IC cases, however, surgical removal of the bladder (Cystectomy) may be inevitable in order to improve patients' quality of life. In these cases, a new bladder can be made from a piece of the patient's intestine that is attached in the place of the removed bladder.
What is the Chronic Pelvic Pain Syndrome?
In contrast to BPS, Chronic Pelvic Pain Syndrome is not always directly related to micturition -even though some urinary problems may exist. Patients report chronic pain in at least two points of the body in the region of pelvis and genitalia. The same testing as mentioned above in BPS is absolutely essential before setting the diagnosis of the Chronic Pelvic Pain Syndrome.
Is there treatment for the Chronic Pelvic Pain Syndrome?
Many pharmaceutical agents -such as antibiotics, antidepressants and natural/plant extracts- as well as physiotherapeutic techniques and acupuncture have been used to treat chronic pelvic pain.