- What is Acute Pyelonephritis?
- What are the symptoms of Pyelonephritis?
- What are the causes of Pyelonephritis?
- How is Pyelonephritis diagnosed?
- How is Pyelonephritis treated?
- What is Chronic Pyelonephritis?
What is Acute Pyelonephritis?
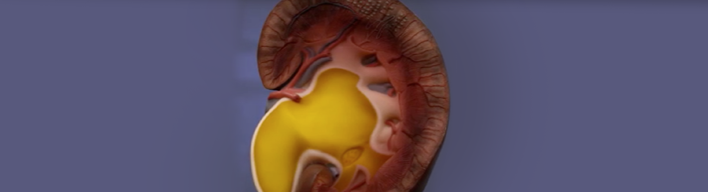
Most urinary tract infections are limited only to the lower urinary tract (urethra and bladder). However, there are cases in which the infection expands also to the upper urinary tract (ureters and kidneys); it is then called Pyelonephritis. Pyelonephritis may potentially evolve to a severe condition because the infection may spread through blood and result in septicemia. But in general, it is almost always a curable disease when administering the appropriate therapeutic regimen. As happens with simple urinary tract infections (UTI), pyelonephritis is also more common in women than men.
What are the symptoms of Pyelonephritis?
Pyelonephritis may initially manifest symptoms similar to those of a simple urinary tract infection (UTI), i.e. urinary frequency and dysuria. However, as the infection spreads to the kidney, the condition becomes more and more severe and further symptoms may emerge, such as:
- Pain in the renal region (usually unilaterally)
- Fever, often with shivering
- Weakness, Fatigue
- Nausea and Vomiting
- Confusion, particularly in the elderly
- In addition, the patient may observe changes in the urine, like the following:
- Hematuria (blood in the urine)
- Cloudy and foul-smelling urine
- Painful urination
What are the causes of Pyelonephritis?
In most cases, bacteria casuing pyelonephritis are the same as those causing simple urinary tract infections (Ε. Coli, Klebsiella etc.). Only rarely may other bacteria -usually located on the skin- immigrate to the kidney through blood and induce pyelonephritis.
There are some conditions predisposing the development of pyelonephritis, such as:
- Diseases preventing the normal urine flow or leading to residual urine. Such most common diseases are Benign Prostasia Hyperplasia, Urolithiasis or some lump in the abdomen and pelvis.
- Diabetes Mellitus, as patients with diabetes are more susceptible to developing infections.
How is Pyelonephritis diagnosed?
The patient's history and clinical examination will help the physician to set the diagnosis of pyelonephritis. It is also important to evaluate the patient's general health condition (blood pressure, pulses, shivering). Then, the doctor will recommend some laboratory tests, such as:
- General urine test (urinalysis) and urine culture, for identifying the microbe responsible for the infection
- General blood test
- Blood culture, for excluding spread of the infection to the blood
- Renal Ultrasound (U/S), for identifying whether there is obstructed urine flow, urolithiasis or abscess formation
- CTscan, giving infomation similar to U/S but in more detail
Besides their contribution to the diagnosis of pyelonephritis, the above screening tests play a significant role in identifying the causes of the disease.
How is Pyelonephritis treated?
Pyelonephritis is a severe infection. It has always to be treated with antibiotics administered for at least 2 weeks. Depending on the patient's general health condition, the physician will decide whether these can be given orally (per os) or whether hospitalization and intravenous administration is required. There are cases when, besides antibiotics, there is also need for some invasive procedure to treat the cause. However, this is avoided, as long as there is active inflammation.
In case there is some obstacle (e.g. ureteral stone), the physician has to intervene in order to restore the normal urine drainage from the kidney. This can be achieved with a tubule (pig-tail) inserted through the bladder reaching up to the kidney. The tubule can be introduced percutaneously with a special needle (percutaneous nephrostomy).
In exceptionally rare cases, the patient's condition may be so much aggravated (immunosupressed, diabetes mellitus patients) that there is need for admission into the Intensive Care Unit (ICU).
What is Chronic Pyelonephritis?
It is a rare disease, which is usually correlated to congenital abnormalities coexisting in the kidneys. It occurs during childhood and recurrent infections result in progressive kidney impairment and scarring. If not treated properly, chronic pyelonephritis may cause even renal failure. Within the context of its treatment, the physician may administer special antibiotics (chemoprophylaxis) for a long period (3-12 months).