- What is the prostate gland?
- Benign Prostatic Hyperplasia/ Hypertrophy (BPH)
- What are the symptoms of BPH?
- What are the implications on the patient's quality of life?
- What happens in BPH?
- How is BPH diagnosed?
- What treatments are available today?
- Surgical Treatments
- The message
All men above the age of 50 will experience some urinary disturbances. Benign Prostate Hyperplasia or Hypertrophy is one of the most common prostatic diseases.
What is the Prostate?
The prostate is a small gland of 3X4 cm, weighing 10-20 gr and having the shape of a chestnut. It is located right below the urinary bladder and above the terminal segment of the intestine, i.e. the rectum. Above the prostate gland are the seminal vesicles which also belong to the reproductive system.
Externally, the prostate gland is coated by a fibromuscular capsule which stretches within the organ and forms pouches. This is the supporting layer of the prostate gland. Inside the gland, there are the glandules that produce the prostatic fluid, which is stored within the gland and ejected during ejaculation by means of muscular contractions of the prostate gland towards the urethra. This is when the neck of the bladder shuts so that the semen does not regurgitate towards the bladder. Through the prostate gland pass the ejaculatory ducts in order to drain into the seminal colliculus, a protuberance of the urethra.
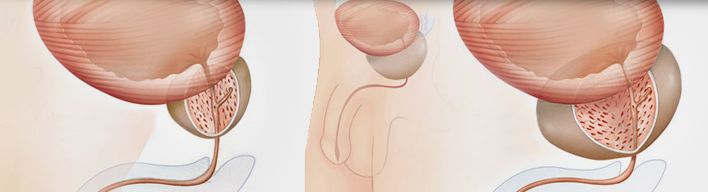
The prostate gland surrounds the terminal segment of the urethra, which is therefore called prostatic urethra and stretches from the seminal colliculus to the neck of the urinary bladder. According to its composition, the prostate gland is divided into zones:
-The transitional zone surrounds the urethra near the bladder and this is the site of hypertrophy in benign prostatic hyperplasia.
-The central zone stretches behind and below the transitional zone and surrounds the ejaculatory ducts.
-The peripheral zone stretches peripherally towards the intestine which is the place of origin of about 80% of prostatic cancers.
And finally, the fibromuscular zone is in front and above the urethra.
In prostate hyperplasia, the enlargement of the transitional zone compresses the others and practically invades the largest part of the gland; in some cases it even penetrates the bladder and, then, we talk about median lobe growth. So, this close prostate-urethra-bladder anatomical relation is responsible for the micturition problems that are related to prostate gland disorders.
Benign Prostatic Hyperplasia/ Hypertrophy (BPS)
Benign prostatic hyperplasia (BPH) is the enlargement of the gland that is observed over the age of 40 years. The increase in the size of the prostate gland frequently compresses the wall of the urethra circularly but also the bladder upwards, inducing micturition disorders which are called ‘lower urinary tract symptoms’ (LURS). It must be underlined that it is not related to prostatic cancer whatsoever, which, unfortunately, does not timely manifest any symptoms.
It is a very common condition, since 4 out of 10 men have symptoms in their 5th decade of life, 7 out of 10 in their 6th decade, 8 out of 10 in their 7th decade, which rate reaches 90% in the 9th decade of life. The condition is more frequently observed in men who are obese, lead a sedentary life, suffer from metabolic syndrome, have erectile dysfunction and an aggravated family history. On the contrary, men with hypogonadism (i.e. testosterone deficiency), rarely present the condition, since the growth of the prostate gland depends on the male hormone.
What are the symptoms of BPS?
Symptoms of micturition disorders -in other words symptoms from the lower urinary tract- are divided into symptoms related to the urine storage and symptoms related to urine voiding from the bladder.
Symptoms related to urine storage in the bladder are the following:
- Frequent micturition (urgent need to urinate even with very small amounts of urine
- Nocturia (nocturnal urination), when we wake up in the night to urinate
- Urinary urgency, when we fail to postpone the need for urination.
- Urge incontinence, when there is an urgent desire to pass urine and sometimes urine leaks before you get to the toilet.
Symptoms related to urine voiding from the bladder are the following:
- Reduction in urine flow and force, due to decreased caliber (diameter) of the urinary stream
- Difficulty to initiate micturition
- Intermittent micturition
- Leak of urine drops after the end of micturition
- Feeling of incomplete bladder voiding
- Total failure to pass urine, the so called urine retention
The only solution to this exceptionally unpleasant situation is the immediate placement of a catheter since the retention pain is unbearable.
Other symptoms are bladder pain, principally during micturition and mainly in cases of urinary tract infection and hematuria (blood in urine) which usually occurs in cases of bladder lithiasis (stones).
What are the implications on the patient's quality of life?
Symptoms of BPH are an immense trouble for both men and their sexual partners, because:
-Their daily professional and social activity is restrained since frequent visits to the toilet cause continuous interruptions.
-Their sleep is troubled, thus, causing a continuous feeling of fatigue.
-Sometimes, they have no time to reach the toilet or even the limited flow of urine becomes the cause of wetting their pants (incontinence).
There is also erectile dysfunction.
Those experiences are accompanied by feelings of shame and humiliation, reduced self-confidence and depressive symptoms. In addition, these problems affect the sexual partner’s quality of life, not only because the couple's sexual life is disrupted but also because the companion is woken and disturbed in the night due to the man’s frequent visits to the toilet and worries watching the partner suffering and sinking into isolation.
What happens in BPH?
In fact, even if the prostate gland is the organ that gets enlarged, it is the urinary bladder that suffers because it is responsible for both the storage of urine and its voiding, i.e. micturition. Thus, in order to be able to overcome the barrier of the prostate gland, the urinary bladder muscle is hypertrophied for exercising more pressure to the urine so that it gets over the obstruction.
In general, we talk about medium glands when they are over 40 gr and large glands when they exceed 80 gr in weight. Of course, this criterion is not an absolute one, since the impact on micturition is determined by the gland’s composition. Thus, a small gland of 20 gr with a fibrous hard composition may cause even urine retention. On the contrary, a smooth prostate gland, even over 100 gr in weight, may cause mild or moderate symptoms. Furthermore, the presence of a middle lobe projecting into the bladder is usually a major problem, since it plays a barrier role to the urine flow.
The hypertrophy of the bladder, however, cannot go on for ever, and so, from a certain point onwards, a quantity of urine remains within the bladder even after micturition; this is called ‘post-void residual urine’. A post-void residual urine quantity over 100 ml is considered pathological since it is indicative of bladder fatigue. Also, the stagnating urine can be easily infected causing urinary tract infections. The existence of post-void residual urine is also a predisposing factor for stone formation within the bladder (lithiasis). Bladder lithiasis may cause pain and frequently hematuria (blood in the urine).
Progressively, however, the residual quantity increases while the thickness of the bladder wall decreases and the bladder is passively distended. Thus, the residual urine quantity increases and may even reach 2 to 3 liters. In such neglected cases, the urine produced in the kidneys cannot descend into the bladder, the renal calyces dilate and lose their shape, causing the so called hydronephrosis (meaning "water inside the kidneys"). If the obstruction remains and no catheter is placed immediately, the renal parenchyma is destroyed and the patient presents renal failure.
How is BPH diagnosed?
The diagnostic process begins with recording the medical history. The type of ailments, their severity, their time of onset and their frequency are basic information that your physician will request to obtain. In order to obtain a better picture of the problem, your physician may ask you to fill in a specific questionnaire. Then a clinical examination is performed including a digital examination of the prostate gland, which is made through the anus [Digital Rectal Examination (DRE) of the Prostate]. It is a basic examination because it provides information about the size of the prostate gland, its composition and any probable suspicion of stiffness in its composition, which is a sign of co-existing prostate cancer.
Furthermore, a basic examination is the measurement of urine flow, i.e. Uroflowmetry. The patient urinates into a special device which measures the urine flow, the quantity voided and the total time of micturition. It is important, after the examination, to establish by use of ultrasounds whether there is residual urine in the bladder. Screening is often completed with renal ultrasonography.
A more detailed screening of the prostate is made through a specific ultrasound probe which is introduced through the rectum and, therefore, it is called Transrectal Prostate Ultrasonography.
After the first visit, the physician may ask you to get a routine urine test and urine culture, along with some blood tests (e.g. urea and creatinine) which indicate the condition of renal function. If you do not have a recent measurement of the prostate-specific antigen, known as PSA contributing to timely diagnosis of prostate cancer, it is certain that the physician will request the test.
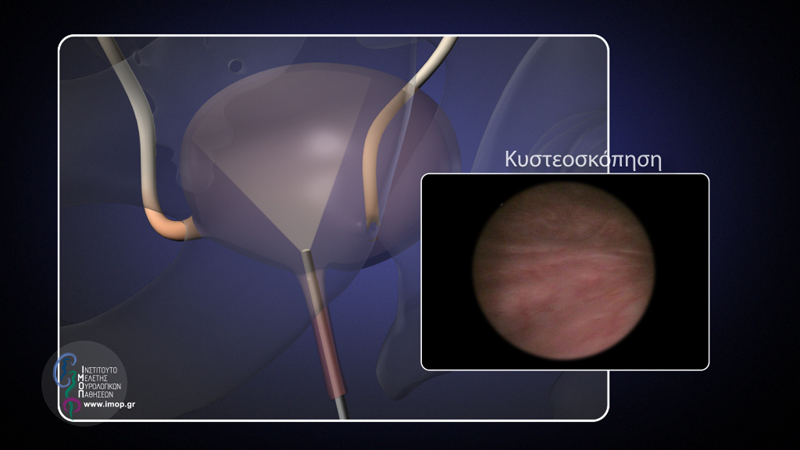
In some cases, an endoscopic examination is performed called Cystoscopy: a small camera mounted at the end of a probe, direct visualization of the urethra, prostate gland and urinary bladder is provided.
Finally, in special cases, tests like radiographic control, upper and lower abdomen CT-scan are performed. Also, Urodynamic Testing which is a special examination studying the urinary bladder and urethral function. The aim of all these tests is for the physician to establish the implications of the condition in order to be able to determine the correct treatment strategy.
What treatments are available today?
Today, there are many therapeutic options providing solution to every man. Your Urologist will recommend to you the most appropriate treatments for your case and will help you opt for one. Let's consider them:
Active monitoring. It is recommended for patients with mild symptoms and minor impact on their daily activities. This therapeutic option includes regular visits to the Urologist and probably some lifestyle changes, such as: control and limitation of fluid intake before going to bed at night, micturition before sleep, abstinence from coffee and alcohol - which have diuretic and irritating action – treatment of any potential constipation control of medications potentially taken by the patient for other conditions which may be aggravating the symptoms. One out of three patients on active monitoring shall not require adjunctive treatment for 5 years.
Medication. In order to determine the most appropriate pharmaceutical treatment for a case, we must know the three factors which determine the symptoms of the patient:
-The first determining factor is the innervation of the prostate gland and urinary bladder. The prostate gland but also the neck of the urinary bladder (the segment of the bladder which is connected to the urethra) have muscular fibers which, through the nerves, can contract and relax. The nerves that are responsible for the contraction are called ‘adrenergic nerves’. At the endings of these nerves a substance - norepinephrin- is released, , which causes contraction of both the urinary bladder neck and prostate gland, when binding on specific receptors called ‘adrenergic receptors’.
The first category of medications used are α-adrenergic receptor blockers ; they are called like that because they bind to adrenergic receptors and, thus, epinephrine is deactivated. Recent data show that these drugs exercise their beneficial action on micturition by activating also some neural pathways outside the prostate gland. A main side-effect of these drugs is a small drop in arterial blood pressure, which is usually manifested as dizziness and weakness, and also as failure to ejaculate.
-The second determining factor is the size of the prostate gland. As the prostate gland grows larger, micturition becomes more and more difficult. The enlargement of the gland is made in the presence of a single hormone called Dihydrotestosterone (DHT). It is produced by the known male hormone testosterone. Testosterone is transformed within the prostate gland into Dihydrotestosterone by the enzyme 5α-reductase. Τhus, in order to decrease the size of the gland and shrink the prostate, 5α-reductase inhibitors are used. Usually, they are given to patients with a prostate gland of over 40 gr in weight and achieve a volume reduction of about 15-25% within 6 months. Probable side-effects may be reduction of sexual desire and erectile dysfunction problems. 5α-reductase inhibitors cause a fictive drop in PSA by even 50%, a fact that must be taken into consideration in the patient’s follow-up. Recently, a pill was introduced into the market combining the two categories of drugs, as it contains an α-blocker (which relaxes the gland) along with the 5α-reductase inhibitor (which shrinks the gland down). This combination treatment has been proven to be the most effective in symptom improvement, prevention of disease progression, urine retention, and, consequently, avoidance of surgery.
-The third determining factor is related to urinary bladder dysfunction. Frequently, the urinary bladder presents innervation disorders resulting in involuntary contractions at urine volumes lower than normal, i.e. less than 400 ml. In this case, we are talking about an Overactive Bladder. Of course, in prostatic hyperplasia, this overactivity is expected, in the context of the bladder’s effort to void. However, when it coexists at pathological levels, then frequent urination, nocturia, and urge get significantly worse in patients with mild obstruction. In such cases, anticholinergic drugs are given together with prostate drugs. They act on the special receptors of the urinary bladder nerves and restrain its involuntary contraction, enabling it to store more urine. Major side-effects of these drugs are xerostomia and constipation. In patients with severe obstruction, they may cause failure in bladder voiding and, rarely, urinary retention.
For the pharmaceutical treatment of prostatic hypertrophy symptoms, herbal medicinal preparations have also been used, such as Serenoa repens and Pygeum africanum. Despite the fact that they have shown positive results, doses of the various products in the market vary and, therefore, must always be taken according to the doctor’s instructions.
Also used is desmopressin, a synthetic analog of the antidiuretic hormone for the treatment of nocturia in patients with high nocturnal urine production. This drug requires special caution when given to men with concomitant cardiovascular problems or to senior patients.
Finally, another drug category, phospho-diesterase 5 inhibitors – known for treating erectional dysfunction – has shown that they safely and effectively improve urinary symptoms in patients suffering from prostatic hyperplasia. Despite the fact that there is no indication for micturition disorders, their daily use seems well- promising for the future for patients with micturition disorders and erectile dysfunction.
Surgical Treatments
We all try to avoid surgery but in some cases an operation becomes necessary. Surgeries for the condition are mainly performed under epidural or spinal anesthesia and the improvement of symptoms is clear right after the operation. It must be underlined that symptom improvement is much higher with surgery than with medication. As in all kinds of surgery, risks for the patients depend on their pre-operative condition and health problems they may potentially have. Prostate surgical procedures are divided into open surgeries, i.e. with an incision and endoscopic methods [through a special endoscope (probe) that is inserted through the urethra]. The most frequent trasnoperative complication is hemorrhage (bleeding); therefore, patients who take anticoagulant drugs and aspirin must discontinue these for several days before surgery. Post-operative complications are urinary tract infections and rarely, retention. After surgery, most men experience a strong urge to urinate and possibly hematuria for 1 to 2 weeks. In most men, retrograde ejaculation is observed postoperatively, which means that although erection and orgasm are not affected, there is no ejaculation. This happens, because the neck of the bladder opens up and the semen goes freely towards the bladder.Urinary incontinence is observed in about 1% of the patients, while the need for revision surgery in the future is not particularly frequent.
Surgical procedures are listed below:
Transurethral Prostatectomy (TURP). Until today it is the most widely used surgical procedure for prostate glands up to 80 gr, even though its popularity has somehow dropped at an international level, due to the development of less invasive methods, such as laser prostatectomy. A special instrument called electrotome (electric cutter) is introduced through the penis to the urethra and reaches the bladder. At its edge there is a special loop that cuts with electrical current the prostate gland into small pieces. At the same time, the spots that are bleeding because of the cuts are cauterized. The tissue fragments that are cut accumulate into the bladder and are removed by washouts with special serum. After the completion of the surgery, a catheter is placed through the urethra which is used for continuous washouts of the bladder in order to avoid blood clotting that might obstruct the catheter. The catheter usually remains for 2-4 days.
Open Prostatectomy. This procedure is performed when the prostate has grown so much - usually over 80 gr - that it does not allow for a safe transurethral prostatectomy. Through an incision made at the lower segment of the abdomen, the gland is removed without its capsule. There are two types of open prostatectomy: Transbladder Prostatectomy, during which the prostate gland is removed through the bladder and Retropubic Prostatectomy, where the capsule is opened and the gland removed. After an open prostatectomy, a catheter is placed into the bladder for 5 to 7 days. The recovery period lasts 4-6 weeks. Complications of open prostatectomy include bleeding; sometimes transfusion is required and, rarely, there is wound infection which is usually superficial.
Laser Transurethral Prostatectomy. It is a technique which, during the 10 past years, has gained in popularity and progressively replaced transurethral and open prostatectomy at an international level. A special instrument is inserted through the urethra under direct visualization and with the use of special optic fibers that are connected to devices producing laser beams of various types. The most tested techniques are those with the use of Holmium laser and green light laser. The Holmium laser is used for prostate gland resection. The gland falls into the bladder and then, with the aid of a special instrument, is dissolved and absorbed. Its results are equal to those of open prostatectomy with lower risk for complications and are, therefore, safer for the patient. The green light laser – so called because of the colour of its laser light beam – is used for selective beam emission on the prostate which is sublimated by the energy of the beam. In all studies the efficacy of these techniques is equal to the efficacy of the classic transurethral prostatectomy. Besides the one and only day of hospital stay, the other main advantage of laser prostatectomy is the absence of bleeding; thus, this method can be used in high risk patients with greater safety, for example in men with severe cardiovascular issues or men receiving anticoagulants. When laser surgery is completed, a catheter is placed through the urethra for 24 hours and the patient is discharged the very next day of the intervention.
The Message
There is no doubt that urinary symptoms due to prostatic enlargement can be treated today in an easy, safe and effective way. Living with the problem is not a solution. A visit to the Urologist will make your everyday life so much easier. There is no reason for delaying this visit; the sooner you visit the Urologist, the better, because timely treatment reduces the chances for any potential future surgery.