Scientific Editor: Editorial Board ISUD website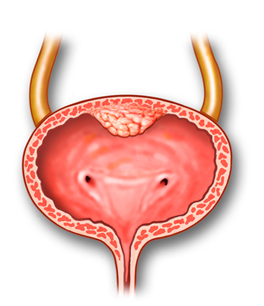
- What is Radical Cystectomy (RC)?
- When is RC performed?
- What preparation is required?
- How is the procedure performed?
- What about after RC?
- How does RC affect patient’s life?
What is Radical Cystectomy (RC)?
When Radical Cystectomy is performed in men, the bladder is removed along with the prostate and seminal vesicles. In women, the bladder is removed along with the uterus, adnexa, urethra and anterior vaginal wall.
When is RC performed?
The procedure is performed in patients with bladder cancer, when biopsy shows that the tumor has invaded the muscle wall and metastasized to other organs. It is also indicated for large or multiple tumors that cannot be removed transurethrally or when bladder haemorrhage cannot be elsewise controlled.
What preparation is required?
Upon hospital admission, the standardized preoperative preparation includes blood tests, chest X-ray and ECG (electrocardiogram). In case you are on anticoagulant therapy, it may be required to interrupt your anticoagulant therapy a few days before the operation. You should always consult your Cardiologist, for there may be need to replace anticoagulants with injections in the abdominal region.
How is the procedure performed?
The procedure is performed under general anaesthesia. In most patients, an epidural catheter is placed to reduce postoperative pain.
Initially, the patient is placed in the supine position and the region is cleansed. An incision is made from just above the umbilicus down to the pubic region. The bladder, surrounding lymph nodes and organs are removed in males and females accordingly, as described above.
Once the bladder is removed, there are various techniques for collecting urine from the kidneys. In most cases the urine is drained through a stoma (opening) created at the patient’s lateral abdominal wall. In other cases, the surgeon uses a short segment of the small intestine to create a new bladder (in the place of the old one) to ensure urinary diversion, so that the patient can urinate through the urethra. At the end of the procedure, a drainage tube (catheter) is placed through the abdominal wall and, in most cases, a nasogastric tube is inserted from the nose to absorb stomach contents. When a new bladder is created with the use of intestinal segment, a second catheter is placed to the bladder through the abdominal region, followed by continuous bladder irrigation. Average length of hospital stay is about 14 days.
What about after RC?
During the first postoperative hours, the patient stays in the Intensive Care Unit (ICU). When back to hospital ward, there is need for the patient’s early feeding and mobilization, to facilitate restoration of intestinal function. Postoperative thrombophylaxis is administered with subcutaneous injections to prevent deep vein thrombosis in the lower extremities or pulmonary embolism. Patients are also trained how to change and take care of the stoma.
Upon discharge, you will be given written instructions about:
- when to obtain histological tissue examination results
- how important it is to drink plenty of fluids
- what sort of nutrition is appropriate
You should necessarily consult your Cardiologist about when to restart anticoagulant treatment.
How does RC affect patient’s life?
Most patients feel fatigue for a period of some months, which is gradually restored. The vast majority of patients will present erectile dysfunction and no patient will be able to have children. Depending on the histological tissue results, there may be need for adjuvant chemotherapy. The patient has to be closely followed up by the Oncologist.


